When an employee gets hurt on the job, the first priority is obvious: physical recovery. A broken wrist, a sprained back, or a chemical exposure comes with medical appointments, treatment plans, and return-to-work timelines. Employers focus on these physical markers because they’re visible, measurable, and required by compliance standards.
But here’s the part that often goes unnoticed: workplace injuries also carry a heavy mental health burden. Anxiety about returning to the same task, depression linked to time away from work, and even post-traumatic stress from the incident itself can quietly linger long after the physical wounds have healed.
For employers, overlooking this hidden dimension comes at a real cost. Workers who struggle silently may take longer to return, underperform when they do, or decide to leave altogether. Productivity drops, turnover climbs, and workers’ compensation claims stretch out. In short, ignoring the mental side of workplace injuries is expensive.
The good news? Employers who shift to a whole-person recovery approach – one that considers both the body and the mind – see faster healing, stronger employee loyalty, and healthier workplace cultures. In this paper, we’ll explore the hidden mental health costs of workplace injuries, why they’re often missed, and how proactive employers can bridge the gap with the right support systems.

The Overlooked Side of Workplace Injuries
When most people think about workplace injuries, they picture the physical damage. A fall on a construction site means broken bones. A strain in a warehouse means pulled muscles. A needlestick injury in a hospital means blood tests and follow-ups. These are the kinds of problems employers are prepared to manage, and they come with clear checklists and compliance requirements.
What often gets overlooked is the mental toll an injury can take. An employee may feel anxious about returning to the same task that caused the injury in the first place. Depression can set in during long recovery periods, especially if the worker feels isolated or worries about job security. Some employees even experience post-traumatic stress, replaying the incident in their mind and struggling with concentration or sleep.
These challenges are not limited to one industry. A truck driver who survives a roadway accident may fear getting behind the wheel again. A healthcare worker injured by a patient may carry lasting stress into every shift. A construction worker who falls from scaffolding may return to work physically healed but mentally unable to climb again.
The truth is that workplace injuries affect both the body and the mind. If employers only address the physical recovery, they are leaving half the problem unsolved. And that half can quietly become the bigger obstacle to getting an employee back to work and thriving again.

The Ripple Effect on Employers
When an injury impacts mental health, it doesn’t just stop with the individual – it ripples through the whole organization. Here’s how:
Extended Recovery Time and Lost Productivity
Injured workers who also face mental health challenges may remain off work up to three times longer than those with purely physical injuries. Even though such cases made up less than 3% of workers’ compensation claims, they accounted for a staggering 35% of total costs. Early mental health intervention is not just compassionate – it’s cost‑effective (Spill, 2025).
In Australia, work-related mental health conditions led to 13% of lost working years, while traumatic injuries and musculoskeletal disorders accounted for 40% and 20.7%, respectively. Annually, this translates to a loss of over 41,000 full-time equivalent jobs, demonstrating the hidden cost of mental health struggles after injuries (Collie et al., 2024).
Absenteeism, Presenteeism, and Health Costs
Mental health issues are a significant driver of absenteeism – 10-15% of all workplace absences are due to mental health-related conditions, and nearly 29% of employees report sick leave for mental health reasons (Gitnux, 2025).
Moreover, employees with high stress and depression can drive healthcare costs up by 200%, and their disability periods can far exceed those associated with other injuries.
Financial Cost and Return on Investment (ROI)
Globally, depression and anxiety cause the loss of around 12 billion working days every year – amounting to a $1 trillion hit to the global economy (Spill, 2025).
But here’s the silver lining: every dollar invested in mental health programs yields about $4.30 in returns (WHO, 2024).
Stress-Related Turnover and Employer Costs
Job stress isn’t just a mood issue – it’s a budget issue. In the U.S., job stress costs companies over $300 billion a year in healthcare costs, absenteeism, disability, turnover, and reduced performance. Businesses with high-stress workers see healthcare costs approximately 50% higher, and turnover driven by stress comprises around 40% of all job turnover (UML / CPH‑NEW data).

Why Employers Miss the Signs
When an injured worker seems physically recovered, it’s easy to assume the rest will just fall into place. But here are some key reasons employers often overlook the mental health side of injury recovery – with data to bring these blind spots into view:
A Culture That Favors Physical over Psychological
While many employers recognize the need to support employees with physical health concerns, mental health remains an afterthought. A 2021 Mental Health America survey revealed that 56% of employees do not view their workplace as a safe or welcoming environment for those living with mental illness – highlighting a gap between intent and reality (Mental Health America, 2021).
Stigma and Employee Concerns
Even when support services exist, employees may hesitate to use them out of fear. A survey by the American Psychiatric Association (APA) found that while 67% of working adults know how to access mental health services at work, around 44% worry about retaliation or being fired if they take time off, and 39% fear retaliation for seeking treatment (APA, 2024).

Lack of Early Recognition
A large disconnect exists between perceived support from leadership and actual employee experience. Employer surveys show that only about 51% report having anti‑stigma or awareness campaigns, while 84% of employees say such campaigns would be valuable. This gap highlights the disconnect between what leaders think they’re communicating and what employees perceive (McKinsey, 2021).
Workplace Culture and Poor Support Structures
Insufficient attention to mental health can have real safety consequences. In Great Britain, analysis by IOSH revealed that poor mental health may contribute to a portion of the 60,645 reported workplace injuries, illustrating how psychological strain can lead directly or indirectly to harm on the job (IOSH, 2023).
Low Psychosocial Safety Climate
Workplaces with poor psychosocial safety climates show higher risks of mental health decline and physical injury. One study in the British Medical Journal found that a poor psychosocial safety climate increased the risk of developing depressive symptoms by up to 200%. Improving that climate could reduce job strain by 14%, depression by 13%, sickness absence by 43%, and presenteeism by 72% – highlighting the impact of culture and organizational environment on wellbeing.
A New Model: Whole Person Recovery
Addressing workplace injuries only through physical treatment is like fixing the frame of a car while ignoring the engine. It may look fine from the outside, but underneath, problems are still slowing things down. A whole-person recovery model acknowledges that injuries affect both the body and the mind, and effective recovery must treat them together.
What Whole-Person Recovery Looks Like
- Integrated Care
- Occupational health providers conduct mental health screenings as part of post-injury evaluations, not just physical checks.
- This can uncover early signs of depression, anxiety, or post-traumatic stress before they derail recovery.
- Access to Support Services
- Employers provide clear pathways to Employee Assistance Programs (EAPs), counseling, and peer-support options.
- Resources are made visible, accessible, and destigmatized, so employees feel safe using them.
- Manager and Supervisor Training
- Supervisors are trained to spot signs of emotional distress – like withdrawal, irritability, or unusual performance dips – so they can connect employees to support.
- Instead of focusing only on compliance or productivity, leaders are equipped to take a human-first approach.
- Gradual Return-to-Work Programs
- Structured return-to-work plans balance physical and psychological readiness.
- Light-duty or phased reintegration can reduce anxiety while building confidence.
Why It Works
The benefits of whole-person recovery extend beyond employee wellbeing:
- Faster recovery timelines: Addressing both mental and physical needs helps employees return to work sooner.
- Higher retention: Workers feel valued and supported, reducing the risk of turnover.
- Stronger safety culture: When employees see that health is prioritized holistically, they are more engaged in safety initiatives.
- Financial ROI: Every dollar invested in mental health support can return more than four dollars in reduced absenteeism, turnover, and healthcare costs.
Putting It Into Place
Organizations that want to embrace whole-person recovery don’t have to reinvent the wheel. By partnering with providers and platforms that are already equipped to handle integrated care, they can close the gaps that currently exist between physical compliance and mental health support.
This is where solutions like BlueHive shine – offering employers the tools to connect employees with the right providers, track both physical and behavioral health, and give HR visibility into overall workforce wellbeing without sacrificing confidentiality.
How BlueHive Supports Employers
Employers do not need to face the challenge of whole-person recovery alone. BlueHive was designed to make health compliance simple while also supporting the broader needs of employees who are recovering from workplace injuries.
Centralized Tracking
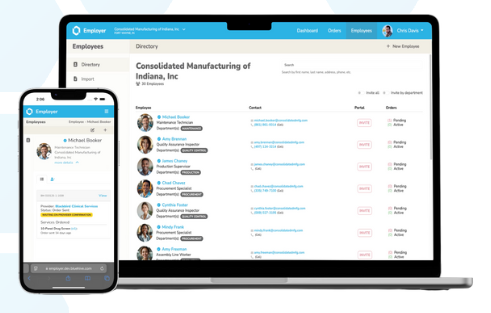
BlueHive gives HR teams and safety leaders a single platform to track both physical and behavioral health assessments. This allows organizations to see patterns and risks across their workforce without sacrificing confidentiality.
A Nationwide Network of Providers
With access to more than 18,000 providers, BlueHive connects employers with occupational health professionals who can address both physical recovery and mental health needs. This means employees are not left to navigate care on their own.
Custom Dashboards for Employers
HR teams gain better visibility into overall workforce wellbeing. BlueHive dashboards provide compliance and health insights in one place, making it easier to spot trends and take proactive steps. Confidentiality is always preserved so employees can feel safe being honest during evaluations.
Improved Communication
Employers, providers, and employees stay connected through secure and customizable portals. This reduces miscommunication, closes gaps in care, and ensures that both physical and mental health needs are addressed as part of the recovery journey.
By combining compliance tracking with true whole-person support, BlueHive helps employers reduce costs, speed up recovery timelines, and foster a culture where employees feel valued and supported.
Conclusion
Workplace injuries affect more than the body. Anxiety, depression, and fear of reinjury can keep employees sidelined long after the physical wounds have healed.
For employers, ignoring this hidden cost leads to longer recoveries, lost productivity, higher turnover, and rising workers’ compensation expenses. The solution is a whole-person recovery approach that integrates mental health screening, accessible support services, and a culture that reduces stigma.
BlueHive makes this possible with centralized tracking, a nationwide provider network, AI-driven documentation support, and employer dashboards. We help organizations move beyond compliance to create workplaces where both body and mind are supported.
Now is the time to act. Employers who embrace whole-person recovery will save on costs and build safer, stronger, and more loyal workforces.
Download the Whitepaper
Sources
- American Psychiatric Association. (2024). New polling data on workplace mental health. Retrieved from https://www.psychiatry.org/news-room/news-releases/new-polling-data-on-workplace-mental-health
- Axios. (2024, May 7). Injured workers need more mental health attention. Retrieved from https://www.axios.com/2024/05/07/injured-workers-mental-health-attention
- Collie, A., Sheehan, L., Lane, T. J., Sim, M. R., & Smith, P. (2024). Work injury and illness costs 41,000 jobs a year. The Australian. Retrieved from https://www.theaustralian.com.au/nation/work-injury-and-illness-costs-41000-jobs-a-year/news-story/2ea96d4cdc387b20e3a03241002c908a
- Gitnux. (2025). Workplace absenteeism statistics. Retrieved from https://gitnux.org/workplace-absenteeism-statistics
- IOSH Magazine. (2023, November 30). Workers with poor mental health take more risks and are more likely to be injured at work, stats reveal. Retrieved from https://www.ioshmagazine.com/2023/11/30/workers-poor-mental-health-take-more-risks-and-are-more-likely-be-injured-work-stats
- McKinsey & Company. (n.d.). National surveys reveal disconnect between employees and employers around mental health need. Retrieved from https://www.mckinsey.com/~/media/McKinsey/Industries/Healthcare%20Systems%20and%20Services/Our%20Insights/National%20surveys%20reveal%20disconnect%20between%20employees%20and%20employers%20around%20mental%20health%20need/national-surveys-reveal-disconnect-around-mental-health.pdf
- Mental Health America. (2021). New OSHA fact sheet outlines workplace mental health concerns. AIHA. Retrieved from https://www.aiha.org/news/240201-new-osha-fact-sheet-outlines-workplace-mental-health-concerns
- Spill. (2025). Workplace mental health statistics. Retrieved from https://www.spill.chat/mental-health-statistics/workplace-mental-health-statistics
- University of Massachusetts Lowell, Center for the Promotion of Health in the New England Workplace. (n.d.). Financial costs of job stress. Retrieved from https://www.uml.edu/Research/CPH-NEW/Worker/stress-at-work/financial-costs.aspx
- Wikipedia. (2025). Occupational stress. In Wikipedia. Retrieved from https://en.wikipedia.org/wiki/Occupational_stress
- Wikipedia. (2025). Psychosocial safety climate. In Wikipedia. Retrieved from https://en.wikipedia.org/wiki/Psychosocial_safety_climate
- World Health Organization. (2024). Mental health at work. Retrieved from https://www.who.int/news-room/fact-sheets/detail/mental-health-at-work




